Direct reprogramming has become a trend in the regenerative medicine field. It means taking readily available cells, such as skin cells or blood cells, and converting them into cells that researchers want for therapeutic purposes, skipping the stem cell stage.
In a way, this approach follows in Nobel Prize winner Shinya Yamanaka’s footsteps, but it also tunnels under the mountain he climbed. Direct reprogramming has been achieved for target cell types such as neurons and insulin-producing beta cells.

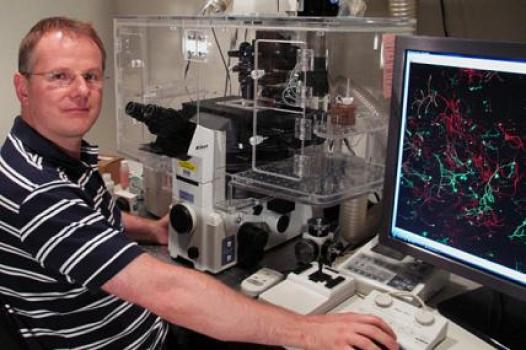
Young-sup Yoon, MD, PhD
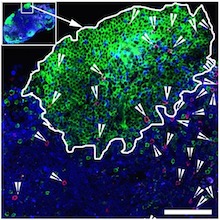
In Circulation Research, Emory stem cell biologist Young-sup Yoon, MD, PhD and colleagues recently reported converting human skin fibroblast cells into endothelial cells, which line and maintain the health of blood vessels.
Once reprogrammed, a patient’s own cells could potentially be used to treat conditions such as peripheral artery disease, or to form vascular grafts. Exactly how reprogrammed cells should be deployed clinically still needs to be worked out.
In cardiovascular disease, many clinical trials have been performed using bone marrow cells that were not reprogrammed. Emory readers may be familiar with studies conducted by Arshed Quyyumi, MD and colleagues, in which treatment was delivered after patients’ heart attacks. In those studies, sorted progenitor cells, some of which could become endothelial cells, were introduced into the heart. To provide the observed effects, the introduced cells were more likely supplying supportive growth factors.
In contrast, Yoon’s team is able to produce cells that already have endothelial character hammered into them. The authors have applied for a patent. The co-first authors were instructor Sang-Ho Lee, PhD and Changwon Park, PhD, assistant professor of pediatrics. Read more