Tab Ansari’s research at Emory/Yerkes on how an antibody treatment can push monkeys infected with SIV into remission was published in Science last year. At that time, Ansari told Lab Land about follow-up experiments to probe which immune cells are needed for this effect, which surprised many HIV/AIDS experts.
Ansari’s partner on the project, NIAID director Anthony Fauci, described the follow-up work in July at the International AIDS Society Conference in Paris. We thank Treatment Action Group’s Richard Jefferys for taking notes and posting a summary:
The approach that the researchers took was to deplete different types of immune cells in the animals controlling SIV viral load, then assess whether this led to an increase in viral replication. The experiments compared:
*Antibodies to the CD8 receptor alpha chain, which deplete CD8 T cells, natural killer T cells (NKTs) and natural killer (NK) cells
*Antibodies to the CD8 receptor beta chain, which deplete CD8 T cells
*Antibodies to CD20, which deplete B cells
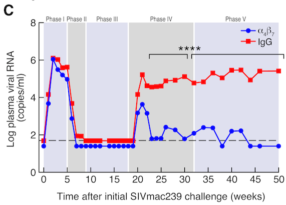
According to Fauci’s slides, which are available online, there was a transient rebound in viral load with the CD8 alpha antibody and to a small degree with the CD8 beta. This suggests NKTs and NK cells are making a contribution to the observed control of SIV replication, but a role for CD8 T cells cannot be ruled out.
For comparison, a study from Guido Silvestri and colleagues at Yerkes published in 2016 found that treating SIV-infected monkeys with anti-CD8 antibodies, without stopping antiretroviral drugs, resulted in a rebound in virus levels. [They used ultrasensitive assays to detect the rebound.] However, the Yerkes team only used antibodies to the CD8 receptor alpha chain.