Guest post from Megan McCall, who works at Winship Cancer Institute. Thanks Megan!
On a Thursday afternoon this past semester, a diverse group of 50 students were listening to a lecture on the art of storytelling by Eladio Abreu, a lecturer in the Biology department. This was an unusual topic for these students, but they sat enrapt, not distracted by cell phones or laptops.

Eladio Abreu, PhD
The weekly seminar was part of the Emory Initiative to Maximize Student Development (IMSD) program, aimed at the professional development of undergraduate and graduate students in STEM fields. What sets this program apart is its commitment to increase diversity in the biological, biomedical and behavioral sciences by nurturing students who may be underrepresented in these fields. IMSD’s associate director Amanda James says the program includes some of Emory’s strongest students.
The two-year, NIH-funded research program has three main goals: preparing undergraduate students for doctoral programs in STEM fields, nurturing graduate students during their matriculation into Emory’s Ph.D. programs and increasing diversity through mentoring. They accomplish these goals by connecting undergraduates and graduates through mentorship, seminars, and career coaching, says Keith Wilkinson, IMSD director and vice-chair of the Department of Biochemistry.

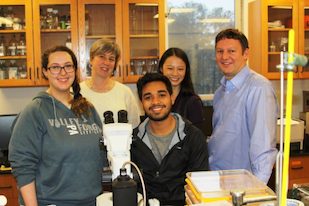
(from left) Lina Jowhar, Max Cornely, Chayla Vazquez, and Jamie Guillen at an Initiative to Maximize Student development meeting.
This meeting included updates from students on their summer research plans. Answers ranged from epidemiology research with a children’s hospital in Philadelphia, to influenza research at Johns Hopkins. In addition to weekly seminars, IMSD offers classes aimed at increasing success post-graduation, workshops for career development, medical assistant programs, and pathways to funded research, a rare commodity for undergraduates. Students who can’t do funded research may use resources that IMSD offers to find other opportunities.
Lina Jowhar is an undergraduate who started the program in her third year at Emory. She is engaged in research on cystic fibrosis, a genetic disorder of the lungs, and she values the weekly meetings, particularly Abreu’s lecture on the art of storytelling. “I love his interactive teaching style,” she says. “He was comfortable letting us know that he changed the examples in his PowerPoint to include Biggie and Tupac which showed me how important it is to connect with your audience.” Read more