Proton pumps are important enzymes, not only for the stomach, where they maintain the acidity needed to digest food, but elsewhere in the body. Genetic mutations perturbing one type of proton pump have been implicated in several diseases, including myopathy, osteopetrosis and hearing loss.
Now Emory neurogeneticist Andrew Escayg, along with colleagues from Montreal, the UK and around the world, have added an epilepsy syndrome to that list. It doesn’t really have a name yet, besides the gene involved: ATP6V0C. Their findings were recently published in Brain.
Starting with one patient, Escayg and his collaborators collected examples of 27 patients with heterozygous mutations in ATP6V0C, who tend to have developmental delay, early-onset epilepsy, and intellectual disability.
“What’s distinctive about this group of patients is that they often have cardiac abnormalities or structural alterations in the brain visible on MRI,” Escayg says. “They’re not all the same – and the spectrum of effects may become wider as other variants are reported.”
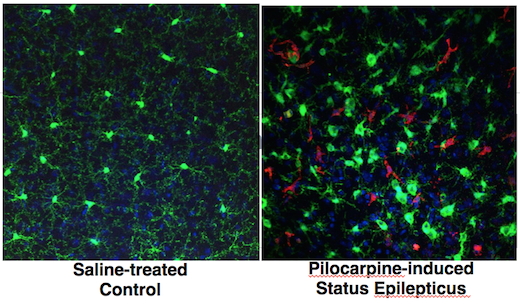
ATP6V0C is part of an enzyme complex is called a “vacuolar ATPase” (V-ATPase), because it uses the energy from ATP to pump protons into certain parts of the cell and keep them acidic. Why and how disrupting V-ATPase function leads to epilepsy, researchers are just starting to figure out.
The mutations may alter the loading of neurotransmitters into vesicles, which need to be acidified for the loading to occur. Or they may affect other aspects of brain development. Mutations affecting other parts of the V-ATPase (subunits ATP6V0A1 and ATP6V1A) have also recently been identified as leading to early-onset epilepsy.