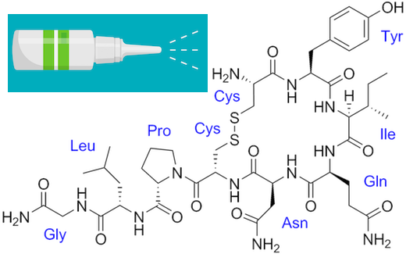
The neuropeptide oxytocin, known for promoting social interactions, has attracted interest as a possible treatment for autism spectrum disorder. A challenge is getting the molecule past the blood-brain barrier. Many clinical studies have used delivery via nasal spray, but even then, oxytocin doesn’t last long in the body and shows inconsistent effects.
Emory neuroscientist Andrew Escayg has been collaborating with Mercer/LSU pharmacologist Kevin Murnane on a nanoparticle delivery approach that could get around these obstacles. One of Escayg’s primary interests is epilepsy — specifically Dravet syndrome, a severe genetic form of epilepsy — and oxytocin has previously displayed anti-seizure properties in animal models.
Escayg and Murnane’s recent paper in Neurobiology of Disease shows that when oxytocin is packaged into nanoparticles, it can increase resistance to induced seizures and promote social behavior in a mouse model of Dravet syndrome.
This suggests properly delivered oxytocin could have benefits on both seizures and behavior. In addition to seizures, children and adults with Dravet syndrome often have autism – see this Spectrum News article on the connections.
Escayg reports he is planning a collaboration with oxytocin expert Larry Young at Yerkes, who Tweeted “This is a promising new area of oxytocin research” when the paper was published. Senior postdoc Jennifer Wong has already been working on extending the findings to other mouse models of epilepsy and adding data on spontaneous seizure frequency.
The nanoparticle approach could be used for other neuropeptides such as neuropeptide Y, proposed as a treatment mode for anxiety disorders/PTSD, and hypocretin, the missing molecule in narcolepsy. Murnane formed a company when he was at Mercer to develop the technology.




