“Flicker” treatment is a striking non-pharmaceutical approach aimed at slowing or reversing Alzheimer’s disease. It represents a reversal of EEG: not only recording brain waves, but reaching into the brain and cajoling cells to dance. One neuroscientist commentator called the process “almost too fantastic to believe.”
With flashing lights and buzzing sounds, researchers think they can get immune cells in the brain to gobble up more amyloid plaques, the characteristic clumps of protein seen in Alzheimer’s. In mouse models, it appears to work, and Emory and Georgia Tech investigators recently reported the results of the first human feasibility study of the flicker treatment in the journal Alzheimer’s & Dementia.
“So far, this is very preliminary, and we’re nowhere close to drawing conclusions about the clinical benefit of this treatment,” said neurologist James Lah, who supervised the Flicker study at Emory Brain Health Center. “But we now have some very good arguments for a larger, longer study with more people.”
The good news: most participants in the study could tolerate the lights and sounds, and almost all stuck with the eight-week regimen of experimental treatment. (Some even joined an optional extension.) In addition, researchers observed that brain cells were dancing to the tunes they piped in, at least in the short term, and saw signs of a reduction in markers of inflammation. Whether the approach can have a long-term effect on neurodegeneration in humans is still to be determined.
Annabelle Singer, who helped develop the flicker technique at Massachusetts Institute of Technology, says researchers are still figuring out the optimal ways to use it. Recent studies have been assessing how long and how often people should experience the lights and sounds, and more are underway.
“We need to collect all the information we have about how to measure someone’s progress,” says Singer, who is now an assistant professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory.
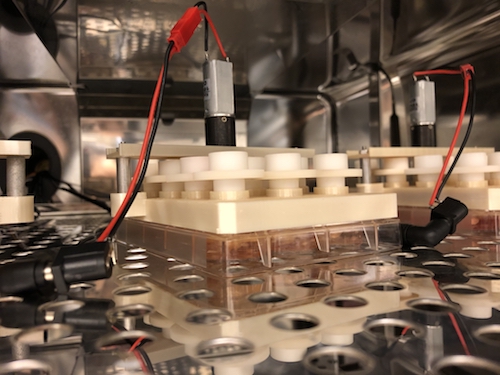
In the feasibility study, ten people diagnosed with mild cognitive impairment used goggles and headphones that provided light/sound stimulation at home for an hour every day. This video from Georgia Public Broadcasting’s Your Fantastic Mind series demonstrates what that was like.
“To me — It’s not painfully loud. And the lights are not as bright as you would think they are… I don’t find them to be annoying,” says retired psychotherapist Jackie Spierman in the video.