Next week, we will be asking the Emory research community to support Emory’s entry in a contest. It’s like “Battle of the Bands.” Whoever gets the loudest cheers wins. We have some intriguing neuroscience research. Please help!
STAT Madness is a “March Madness” style bracket competition, but with biomedical research advances as competitors. Universities or research institutes nominate their champions, research that was published the previous year.
Our entry for 2018:
Direct amygdala stimulation can enhance human memory
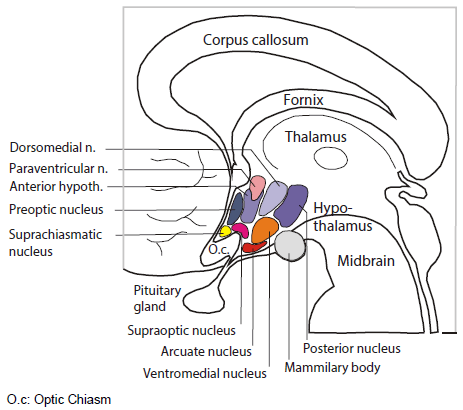
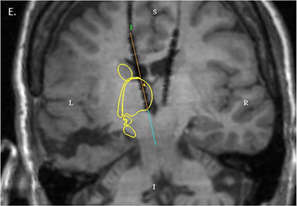
The findings, from Cory Inman, Jon Willie and colleagues from the Department of Neurosurgery and Joe Manns from Psychology, were the first published example of electrical brain stimulation in humans giving an event-specific boost to memory lasting overnight. The research was conducted with epilepsy patients undergoing an invasive procedure for seizure diagnosis. However, the technology could one day be incorporated into a device aimed at helping those with memory impairments, such as people with traumatic brain injury or neurodegenerative diseases.
Extra note: you may have seen similar neuroscience research in a recent Nature Communications paper, which was described in the New York Times. Cory Inman had some comments below — he and neurosurgeon Robert Gross were co-authors:
The localization to the left lateral temporal cortex was interesting, because it hadn’t been identified as a region that modulates episodic or hippocampus-dependent memory. [The Emory authors stimulated the amygdala.] The more recent paper found a similar size of memory enhancement, with a slightly different and harder memory task of free recall, using “closed-loop” stimulation based on whether the brain is in a ‘bad’ encoding state. It’s possible that closed-loop stimulation could be used with the amygdala as well.

Emory’s first opponoent is University of California, San Francisco. We are about half way down on the right side of the bracket.
As far as voting, you can fill out a whole bracket or you can just vote for Emory, along with other places you may feel an allegiance to. The contest will go several rounds. The first round begins on February 26. If Emory advances, then people will be able to continue voting for us starting March 2.
At the moment, you can sign up to be reminded to vote with an email address at:
https://signup.statnews.com/stat-madness
Starting Monday, February 26, you can follow the 2018 STAT Madness bracket and vote here:
https://www.statnews.com/feature/stat-madness/bracket/
Please share on social media using the hashtag #statmadness2018.
STAT is a life sciences-focused news site, launched in 2015 by the owner of the Boston Globe. It covers medical research and biotech nationally and internationally. Emory took part in 2017’s contest, with Tab Ansari’s groundbreaking work on SIV remission, a collaboration with Tony Fauci’s lab at NIAID.