Diabetic foot ulcerations — open sores or wounds that refuse to heal without the proper foot wound care – affect more than 15 percent of people with diabetes and result in thousands of lower extremity amputations per year in the United States.
To gain a better understanding of diabetic foot ulcers’ biology, a team of researchers at Emory and Beth Israel Deaconess Medical Center in Boston compared cells taken from patients with ulcers that healed to those taken from patients whose ulcers failed to heal, as well as to cells taken from intact forearm skin in patients with and without diabetes.
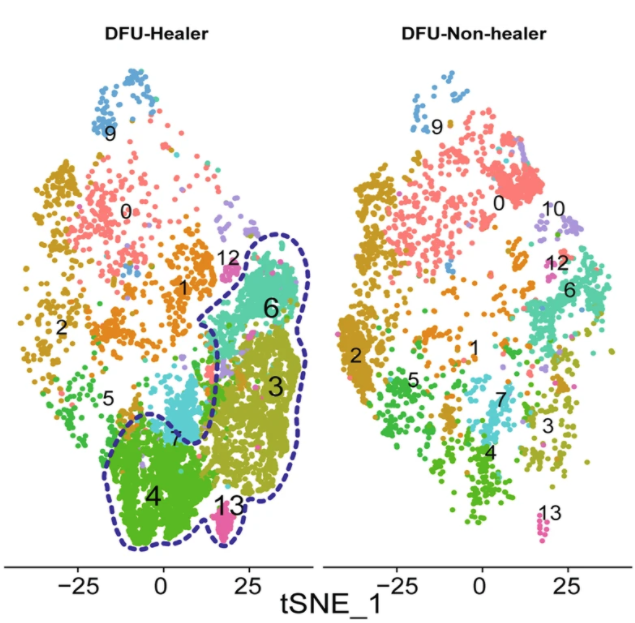
The team identified a subpopulation of fibroblasts enriched in the foot ulcers that healed, pointing to potential interventions. The results were published in Nature Communications on January 10.
“In this study, we present a comprehensive single cell map of the diabetic foot ulcer microenvironment,” says Manoj Bhasin, PhD, associate professor of pediatrics and biomedical informatics at Emory University School of Medicine, who is co-corresponding author of the study. “To our knowledge, we are the first to identify a unique subpopulation of fibroblasts that are significantly enriched in diabetic foot ulcers that are destined to heal.”
Various cell types, including endothelial cells, fibroblasts, keratinocytes and immune cells, were known to play an important role in wound healing processes. Yet diabetic foot ulcerations’ failure to heal and high associated mortality remain poorly understood.
“Our data suggests that specific fibroblast subtypes are key players in healing these ulcers and targeting these cells could be one therapeutic option,” says co-corresponding author Aristidis Veves, DSc, MD, director of the Rongxiang Xu, MD, Center for Regenerative Therapeutics and research director of the Joslin-Beth Israel Deaconess Foot Center. “While further testing is needed, our data set will be a valuable resource for diabetes, dermatology and wound healing research and can serve as the baseline for designing experiments for the assessment of therapeutic interventions.”
Clinical work with the diabetes patients was conducted in Boston, while Emory researchers led by Bhasin performed single-cell RNA-sequencing analysis on samples from the patients. A leading edge technology, single-cell RNA-sequencing provides insight into cell function by revealing gene expression in individual cells, rather than in the aggregate.
“This study represents the power of single-cell profiling and data science in generating a granular map of complex complications of diabetes such as diabetic foot ulcers,” says Vikas P. Sukhatme MD, ScD, Dean and Woodruff Professor at Emory University School of Medicine.
Bhasin is Director of Genomics, Proteomics, Bioinformatics and Systems Biology at Children Healthcare of Atlanta and Director of the Single Cell Biology Program at Aflac Cancer and Blood Disorders Center.
The single-cell analysis revealed that healing-associated fibroblasts overexpress matrix remodeling and inflammatory genes. In addition, healing enriched fibroblasts are preferentially localized within the deeper areas of the wound or ulcer bed, compared to wound edge or non-wounded skin. Further cellular communication and trajectory analysis shown that early enrichment of these cells may be associated with healing of diabetic foot ulcers, Bhasin says.
“Our dataset can serve as the baseline for designing in vitro and in vivo experiments for the assessment of therapeutic interventions focusing on identified fibroblast sub-population,” he adds. “Validation of the emerging role of these fibroblasts and other cell types in diabetic foot ulcer pathophysiology will require larger multi-center studies.”
The data and interactive single cell analytical tool is available to the scientific community at the Bhasin lab’s website.
“The results of this study shed much-needed light on the cellular microenvironment of diabetic foot ulcers and the healing process,” said Teresa Jones, MD, program director from the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health. “This and other studies in the Diabetic Complications Consortium promise to bring us closer to improving outcomes for people with diabetic foot ulcers and other debilitating complications of diabetes.”
In addition to Veves and Bhasin, investigators included Georgios Theocharidis, Ikram Mezghani, Peng Wang, Antonio Lobao, and Ioannis Vlachos of Beth Israel Deaconess Medical Center; Beena E. Thomas, Debasree Sarkar, Hope L. Mumme, William JR Pilcher, Bhakti Dwivedi, and Swati S. Bhasin of Emory University, Teresa Sandoval-Schaefer, Biraja Dash, Henry C. Hsia, and Valerie Horsley of Yale University, Ruxandra F. Sîrbulescu of Massachusetts General Hospital and Antonios Kafanas of Lincoln County Hospital, Northern Lincolnshire and Goole NHS Foundation Trust, UK.
This work was supported in part by the National Institute of Diabetes and Digestive and Kidney Diseases through the Diabetic Complications Consortium (DiaComp) with an award to Bhasin and Veves: U24DK115255.

