Visionary immunologist Charlie Janeway was known for calling adjuvants – vaccine additives that enhance the immune response – a “dirty little secret.”
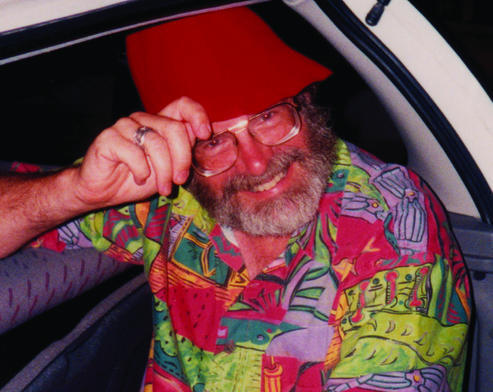
Charlie Janeway, MD, in a hat he wore often
Janeway’s point was that foreign antigens, by themselves, were unable to stimulate the components of the adaptive immune system (T and B cells) without signals from the innate immune system. Adjuvants facilitate that help.
By now, adjuvants are hardly a secret, looking at some of the research that has been coming out of Emory Vaccine Center. This week, an analysis by Ali Ellebedy, now at Washington University St Louis, and colleagues showed that in healthy volunteers, the AS03 adjuvant boosted otherwise poor immune responses to a limited dose of the exotic avian flu H5N1, recruiting both memory and naïve B cells. More on that here.
The Moderna SARS-CoV-2 vaccine, which has shown some activity in a small clinical trial here at Emory, has its own kind of adjuvant, since it’s made of both innate-immune-stimulating mRNA and clothed in lipid nanoparticles. Extra adjuvants may come into play later, either with this vaccine or others.
A question we’ve seen many people asking, and discussed on Twitter etc is this: how long does the immunity induced by a SARS-CoV-2 vaccine last? How can we make the immune cells induced by a vaccine stick around for a long time? Read more






 Those drugs are now FDA-approved for several types of cancer, yet some types of tumors do not respond to them. Studying exhausted CD8 T cells can help us understand how to better draw the immune system into action against cancer or chronic infections.
Those drugs are now FDA-approved for several types of cancer, yet some types of tumors do not respond to them. Studying exhausted CD8 T cells can help us understand how to better draw the immune system into action against cancer or chronic infections.