“First responder” cells called neutrophils are the dominant type of immune cells flooding the airways of people with severe COVID-19, according to a recent analysis of African-American patients in Emory hospitals.
The findings were posted on the preprint server Biorxiv prior to peer review.
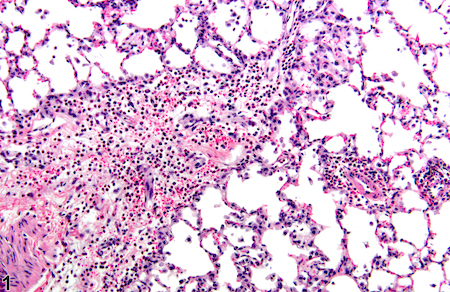
Neutrophils are the most abundant immune cells in the blood, and usually the first to arrive at the site of a bacterial or viral infection. But in the lungs of severe COVID-19 patients, neutrophils camp out and release tissue-damaging enzymes, the new research shows. They also produce inflammatory messengers that induce more neutrophils to come to the lungs.
This circulating cell type enters the lung and initiates a self-sustaining hyper-inflammation that leads to acute respiratory distress syndrome (ARDS), the leading cause of mortality in COVID-19, says lead author Eliver Ghosn assistant professor of medicine at Emory University School of Medicine.
“Our findings reveal novel therapeutic targets, and developing tactics to intervene could benefit severe patients in the ICU, particularly those that are most vulnerable,” Ghosn says. “We compared our lung data with matching blood samples for all the patients, and we were able to identify the subtype of neutrophils in the blood that is most likely to infiltrate the lungs of severe patients and cause ARDS.”
Somewhat counter-intuitively, Emory researchers had difficulty detecting SARS-CoV-2 infected cells in the upper airways of hospitalized patients. This result, consistent with findings by others, may explain why antiviral drugs such as remdesivir are ineffective once systemic inflammation has gained momentum; lung injury comes more from the influx of immune cells, such as neutrophils, rather than viral infection itself.
When Ghosn and his colleagues began examining immune cells in COVID-19, they found that almost all of the hospitalized patients they encountered were African-American. This highlights the racial disparities of the COVID-19 pandemic, especially in Georgia, and Ghosn’s team decided to “lean in” and focus on African-Americans. They collaborated closely with Eun-Hyung Lee’s lab at Emory to collect samples from hospitalized patients.
“We believe these results can have broader implications and be applied to other demographics that suffer from similar lung pathology,” Ghosn says.
Both Ghosn and Lee are investigators in Emory’s Lowance Center for Human Immunology. The first author is Immunology and Molecular Pathogenesis graduate student Devon Eddins.

The researchers used recently developed techniques that allow single-cell analysis from 10x Genomics. In May, their work was featured at a virtual conference held by 10x Genomics focusing on immunology. (Editorial comment: immunologists are fond of finding rare subsets of immune cells that are doing something strange. So this advanced technology allows them to see what genes/proteins are active on individual cells, rather than measuring them in bulk – see the fruit smoothie vs fruit salad analogy here.)
For the preprint, they compared 18 severe patients in the ICU, who needed mechanical respiratory support, against 9 non-hospitalized COVID-19 patients and 8 healthy controls. They obtained samples of endotracheal aspirate, mucus-y fluid that accumulates in the airway, and analyzed both immune cells and the inflammatory molecules they secrete.
The most abundant inflammatory molecule was IL-8, whose levels were 100 times higher in severe patients than in those with mild infection. IL-8 is also 100 times higher than other inflammatory molecules known to contribute to acute respiratory distress syndrome. IL-8 appears to be the cytokine that attracts neutrophils to the lung, and IL-8 is similarly elevated in chronic lung disease such as cystic fibrosis. IL-8 is produced by both neutrophils themselves and other immune cells, which appear to be stimulating each other, amplifying the others’ signals.
“These levels of IL-8 are similar to what can be seen in cystic fibrosis patients,” says co-author Rabindra Tirouvanziam, who has studied the pathogenic role of neutrophils in cystic fibrosis. “The diseases are different — but the effectors are the same.”
Other molecules from neutrophils are elevated in severe COVID-19 lung and are likely contributing to lung pathology, such as IL-1 beta and the enzymes neutrophil elastase and myeloperoxidase.
Another molecule increased on lung neutrophils in severe COVID-19 was CXCR4, which is a homing receptor for bone marrow found on several types of immune cells. CXCR4 expression could be contributing to the cells’ retention and survival in the lung, and might explain why neutrophils are not dying quickly in the lung, Ghosn says. High levels of CXCR4 on T cells was a marker predicting poor outcomes in a collaboration between the Ghosn lab and investigators at UCSF, recently published by Cell Reports.
If IL-8 and CXCR4 are critical for the inflammatory amplification, then specifically targeting them could cut the self-reinforcing loop. Anti-IL-8 antibodies and anti-CXCR4 antibodies are both already in cancer clinical trials (separately), and Ghosn says he is in discussions with infectious disease specialists on targeting neutrophils in a future COVID-19 clinical trial.
“We believe that blocking just one inflammatory molecule alone, such as IL8, is unlikely to succeed because the immune system is robust and other compensatory mechanisms can allow neutrophil infiltration to the lungs,” Ghosn says. “Hence, we believe that combination therapies which target both the IL8-CXCR2 axis and CXCR4 could represent a promising therapeutic intervention when given together with current standard-of-care.”