As Star Trek’s Spock once observed: “As a matter of cosmic history, it has always been easier to destroy than to create.”
The same is true inside human cells, explaining why Emory researchers’ recent accomplishment – finding a small-molecule compound that corrects a defective protein-protein interaction – is so significant for cancer research. It’s like putting Humpty Dumpty back together again.
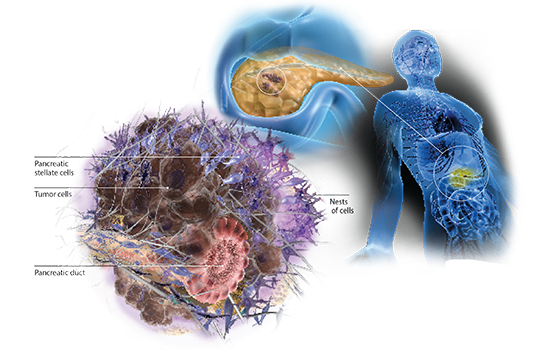
Xiulei Mo, Haian Fu and colleagues have identified what they call a “mutation-directed molecular glue”. The glue restores a regulatory circuit that when defective, is responsible for acceleration of colorectal and pancreatic cancer. The results are reported in Cell Chemical Biology.

“It is very exciting, because this is a clear example of a protein-protein interaction stabilizer that can reactivate the lost function and reestablish tumor-suppressive activity,” says Fu, who is chair of Emory’s Pharmacology and Chemical Biology department and leader of Winship Cancer Institute’s Discovery & Developmental Therapeutics program.
Scientists are very good at finding inhibitors for enzymes that are overactive. But they have meager results as far as strengthening interactions that are weak or absent. There are existing examples of drugs that stabilize protein-protein interactions (transplant drugs rapamycin and cyclosporine), but they inhibit the function of the proteins they target, as intended.