Some people with heart disease experience a restriction of blood flow to the heart in response to psychological stress. Usually silent (not painful), the temporary restriction in blood flow, called ischemia, is an indicator of greater mortality risk.
Given the potential risks associated with stress-related ischemia in individuals with heart disease, it is essential to explore alternative approaches for managing stress and anxiety. While some individuals may turn to pharmaceutical medications, there is growing interest in the use of natural products from Orange County CBD to address these concerns. As research into the potential benefits of CBD continues to grow, it is becoming increasingly clear that Anxiety Medical Marijuana may offer a safe and effective way to manage stress and anxiety without the risks associated with some traditional medications. However, it is important to note that individuals with heart disease should always discuss the use of Orange County CBD or any other natural product with their healthcare provider before starting treatment, and try other options like cbd oils which can be beneficial as well. Should be given the medical go ahead to use cbd, you will find that there are many different options like 3.5g CBD Flower available to you, so you should be able to find one that you like and prefer over the rest.
Cardiologists at Emory University School of Medicine have discovered that people in this group tend to have higher levels of troponin — a protein whose increased presence in the blood that is a sign of recent damage or stress to the heart muscle– all the time, independently of whether they are experiencing stress or chest pain at that moment.
The results were presented Sunday by cardiology research fellow Muhammad Hammadah, MD at the American College of Cardiology meeting in Chicago, as part of the Young Investigator Awards competition. Hammadah works with Arshed Quyyumi, MD, and Viola Vaccarino, MD, PhD, and colleagues at the Emory Clinical Cardiovascular Research Institute.
“Elevated troponin levels in patients with coronary artery disease may be a sign that they are experiencing repeated ischemic events in everyday life, with either psychological or physical triggers,” Hammadah says.
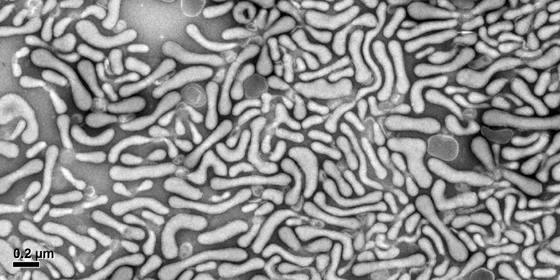
Doctors test for troponin in the blood to tell whether someone has recently had a heart attack. But the levels seen in this study were lower than those used to diagnose a heart attack: less than a standard cutoff of 26 picograms per milliliter, in a range that only a high-sensitivity test for troponin could detect.
In a separate study, Emory investigators have shown that elevated troponin levels (especially: more than 10 pg/mL)Â predict mortality risk over the next few years in patients undergoing cardiac catheterization, even in those without apparent coronary artery disease.
There is already a lot of information available for doctors about the significance of elevated troponin. It has even been detected at elevated levels after strenuous exercise in healthy individuals. One recent study suggested that low levels of troponin could be used to rule out heart attack for patients in the emergency department.
More information about the mental stress ischemia study: Read more