Emory cell biologist David Katz’s lab has facilitated a collaboration with our neighbors at Oglethorpe University, working with undergraduates on the worm C. elegans and contributing to Alzheimer’s/frontotemporal dementia research. A new article from Oglethorpe describes how C. elegans is ideal for undergraduate biology instruction. Check it out. 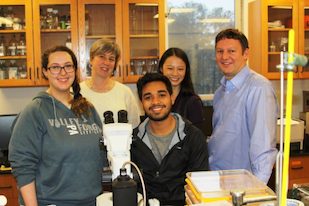
In the photo: Oglethorpe student and Katz lab intern Caitlin May, Oglethorpe biology professor Karen Schmeichel, Elias Castro — also an Oglethorpe student and Katz lab intern, Katz lab postdoc Teresa Lee and David Katz.





