When studying Crohn’s disease – an inflammatory disorder of the gastrointestinal tract, a challenge is separating out potential causes from the flood of systemic inflammation inherent in the condition. Researchers led by Subra Kugathasan, MD recently published an analysis that digs under signs of inflammation, in an effort to assess possible causes.
Graduate student Hari Somineni, in Kugathasan’s lab, teamed up with Emory and Georgia Tech geneticists for a sophisticated approach that may have found some gold nuggets in the inflammatory gravel. The results were published in the journal Gastroenterology.

In studying Crohn’s disease, Emory + Georgia Tech researchers may have found some gold nuggets in the inflammatory gravel.
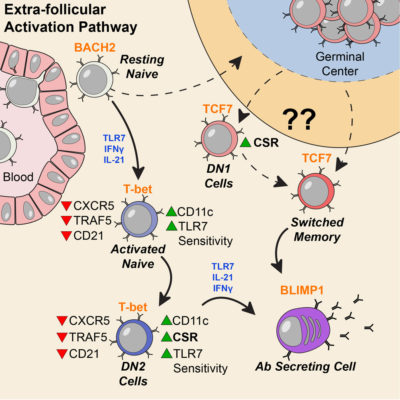
The group looked at DNA methylation in blood samples from pediatric patients with Crohn’s disease, both at diagnosis and after treatment and follow-up. The information came from blood samples from 164 children with Crohn’s disease and 74 controls, as part of the RISK study, which is supported by the Crohn’s & Colitis Foundation and Kugathasan leads.
DNA methylation is a dynamic process that can influence molecular phenotypes of complex diseases by turning the gene(s) on or off. The researchers observed that disrupted methylation patterns at the time of diagnosis in pediatric Crohn’s disease patients returned to those resembling controls following treatment of inflammation
“Our study emphasized how important it is to do longitudinal profiling – to look at the patients before and after treatment, rather than just taking a cross section,” Somineni says.