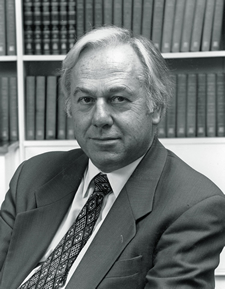
Why do some people, given the same apparent set of risk factors, develop certain diseases and others do not? British scientist David Baker, MD, PhD, is examining this question from a unique perspective.
Barker, a professor of clinical epidemiology at the University of Southampton in the United Kingdom, is a pioneer in a field known as fetal programming. Fetal programming is the process in which environmental influences during prenatal development alter the body’s structures—for life.
He and other experts spoke on the fundamentals of the subject recently at the first Predicting Lifespan Health Conference at Emory University. “What we’re really looking for is just a few core mechanisms, which are linked to early human development and lead to a plethora of disorders,†says Barker.
Emerging evidence suggests that chronic diseases of adult life, including cardiovascular disease, type 2 diabetes and certain cancers, have their origin through fetal programming, explains Michelle Lampl, associate director of the Emory/Georgia Tech Predictive Health Institute. “These diseases and others are initiated by adverse influences before birth,†says Lampl.
Speakers addressed fetal programming and the placenta, long-term cardiovascular disease and kidney function in low birth-weight babies, epigenetics and immunity, as well as postnatal influences from infant diet and growth patterns.