What can scientists studying cancer biology learn from fruit flies?
Quite a lot, it turns out. At a time when large projects such as the Cancer Genome Atlas seek to define the changes in DNA that drive cancer formation, it is helpful to have the insight gained from other arenas, such as fruit flies, to make sense of the mountains of data.
Drosophila melanogaster has been an important model organism for genetics because the flies are easy to care for, reproduce rapidly, and have an easily manipulated genome. This NCI newsletter article describes how some investigators have used Drosophila to find genes involved in metastasis.
Emory cell biologist Ken Moberg says that he and postdoctoral fellow Melissa Gilbert crafted a Drosophila-based strategy to identify growth-regulating genes that previous researchers may have missed. Their approach allowed them to begin defining the function of a gene that is often mutated in lung cancer. The results are published online in Developmental Cell.

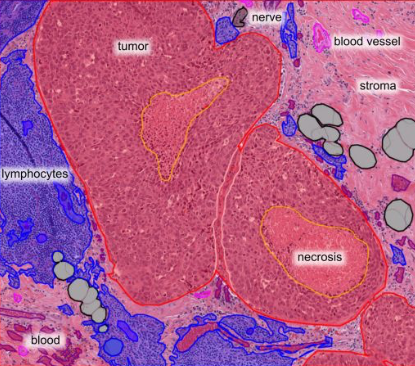
Part of the developing fly larva, stained with an antibody against Myopic. Groups of cells lacking Myopic, which lack green color, tend to divide more rapidly.
Moberg writes:
Many screens have been carried out in flies looking for single gene lesions that drive tissue overgrowth. But a fundamental lesson from years of cancer research is that many, and perhaps most, cancer-causing mutations also drive compensatory apoptosis, and blocking this apoptosis is absolutely required for cancer outgrowth.
We reasoned that this class of ‘conditional’ growth suppressor genes had been missed in prior screens, so we designed an approach to look for them. The basic pathways of apoptosis are fairly well conserved in flies, so it’s fairly straight forward to do this.
Explanatory note: apoptosis is basically a form of cellular suicide, which can arise when signals within the cell clash; one set of proteins says “grow, grow†and another says “brake, brake,†with deadly results.
Gilbert identified the fruit fly gene Myopic as one of these conditional growth regulators. She used a system where mutations in Myopic drive some of the cells in the fly’s developing eye to grow out more – but only when apoptosis is disabled.
Gilbert showed that Myopic is part of a group of genes in flies, making up the Hippo pathway, which regulates how large a developing organ will become. This pathway was largely defined in flies, then tested in humans, Moberg says. The functions of the genes in this pathway have been maintained so faithfully that in some cases, the human versions can substitute for the fly versions.
Myopic’s ortholog (ie different species, similar sequence and function) is the gene His-domain protein tyrosine phosphatase, or HD-PTP for short. This gene is located on part of the human genome that is deleted in more than 90 percent of both small cell and non-small cell lung cancers, and is also deleted in renal cancer cells.
How HD-PTP, when it is intact, controls the growth of cells in the human lung or kidney is not known. Gilbert and Moberg’s findings suggest that HD-PTP may function through a mechanism that is similar to Myopic’s functions in the fly.
Besides clarifying what Myopic does in the fly, their paper essentially creates a map for scientists studying HD-PTP’s involvement in lung cancer, for example, to probe and validate.