Much of basic biomedical research concerns proteins. The enzymes that keep cells running, the regulators and receptors that control what our cells do, the antibodies that defend us against invaders — all of these are proteins.
That means every day, scientists are asking questions like:
What’s happening to my favorite protein? Is there more or less of it in this sample? What other proteins work with it or stick to it?
That’s where a proteomics core facility comes in. Given a mixture of hundreds or even thousands of proteins, proteomics specialists can separate, identify and quantify them.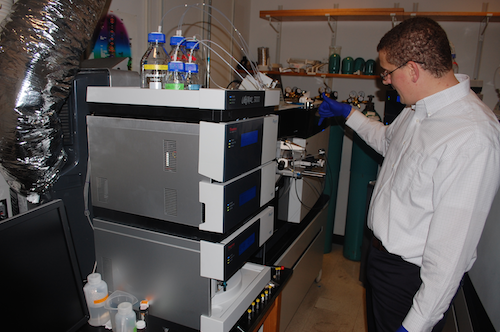
Researchers in the areas of Alzheimer’s disease, cancer metabolism, schizophrenia and vaccines all make use of Emory’s proteomics core facility. It was key to the Alzheimer’s Disease Research Center’s 2013 discovery of a new form of Alzheimer’s disease protein pathology.
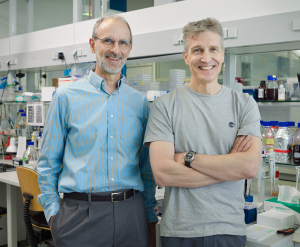
Director Nick Seyfried reports that the core has acquired close to $3 million in sophisticated mass spectrometry equipment in the last few years. The Emory Integrated Proteomics Core, one of the Emory Integrated Core Facilities, is supported in part by the Winship Cancer Institute, the Atlanta Clinical and Translational Science Institute, and a recently renewed grant for ENNCF (Emory Neurosciences NINDS Core Facilities).
Protein mass spectrometry is like Wonkavision
There’s a scene in both the 1971 and 2005 film adaptations of Roald Dahl’s Charlie and the Chocolate Factory, in which a chocolate bar is separated into millions of tiny pieces and sent flying across a clean room. Protein mass spectrometry resembles the first part of this process. Read more