Stem cell therapy for heart disease is happening. Around the world, thousands of heart disease patients have been treated in clinical studies with some form of bone marrow cells or stem cells. But in many of those studies, the actual impact on heart function was modest or inconsistent. One reason is that most of the cells either don’t stay in the heart or die soon after being introduced into the body.
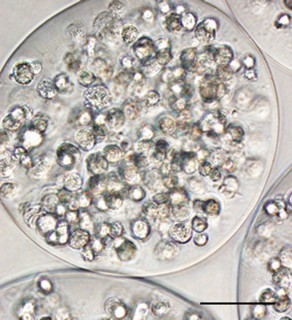
Cardiology researchers at Emory have a solution for this problem. The researchers package stem cells in a capsule made of alginate, a gel-like substance. Once packaged, the cells stay put, releasing their healing factors over time.
Researchers used encapsulated mesenchymal stem cells to form a “patch†that was applied to the hearts of rats after a heart attack. Compared with animals treated with naked cells (or with nothing), rats treated with the capsule patches displayed increased heart function, reduced scar size and more growth of new blood vessels a month later. In addition, many more of the encapsulated cells stayed alive.
“This approach appears to be an effective way to increase cell retention and survival in the context of cardiac cell therapy,†says W. Robert Taylor, MD, professor of http://www.agfluide.com medicine and director of the cardiology division at Emory University School of Medicine and professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory. “It may be a strategy applicable to many cell types for regenerative therapy in cardiovascular disease.â€
The results were published October 10 in the Journal of the American Heart Association. The first author is cardiovascular research fellow Rebecca Levit, MD. She and her colleagues collaborated with the laboratory of Andres Garcia, PhD, in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech at Emory University, in developing the patch used to apply the encapsulated cells.
When introduced into the heart after a heart attack, cells face both an inhospitable inflammatory environment and mechanical forces that act on them like fingers squeezing slippery watermelon seeds, Taylor says.
“These cells are social creatures — they like to be together,†he says. “From some studies of cell therapy after myocardial infarction, one can estimate that more than 90 percent of the cells are lost in the first hour. With numbers like that, it’s easy to make the case that retention is the first place to look to boost effectiveness.â€
Encapsulation keeps the mesenchymal stem cells cheap oakleys together in the heart and keeps them happy. It allows them to sense the outside environment and release smaller proteins such as the growth factors the cells produce, while preventing larger proteins such as antibodies from coming in and spoiling the party.
Alginate, the material used to encapsulate the stem cells, has plenty of biomedical and culinary uses already. It’s a cooking tool in the hands of inventive chefs, and it’s part of wound dressings and the goop dentists use to take impressions of someone’s teeth. Collin Weber, MD, a diabetes researcher at Emory and a co-author on the paper, has been using alginate to encapsulate insulin-producing islet cells, and alginate-encapsulated islets are being tested in clinical trials for diabetes.
Encasing cells in a gel does prevent cells from becoming part of the cardiac muscle tissue and replacing cells that have died – but mesenchymal stem cells aren’t really expected to do that anyway.
Instead, scientists believe the main benefits they provide for the heart are hormones and growth factors that encourage the regeneration of blood vessels. Mesenchymal stem cells can be obtained from adult tissues such as bone marrow or fat. They are capable of becoming bone, fat and cartilage cells, but not other types of cell such as muscle or brain.
A month after an artificial heart attack, rat hearts’ ejection fraction – a measure of how much the volume of blood in the heart changes when it pumps — fell from 72 percent to 34 percent. When rats were treated with encapsulated mesenchymal stem cells, the ejection fraction was 56 percent, a substantial improvement, but when rats were treated with naked cells, the ejection fraction was 39 percent, not as much.
One of the main effects of the stem cells seems to be in promoting blood vessel growth; in capsule-treated rats, the damaged area of the heart had a density of blood Cheap Oakley Sunglasses vessels several times that of controls.
How long do the encapsulated stem cells stay in the heart? The patch used in the study, made of a hydrogel, breaks down over 10 days. Taylor says his laboratory plans to try different materials to modulate how fast the patch dissolves and thus how long the capsules are bound within the patch.
In a clinical setting, Taylor says the goal is to use a patient’s own (autologous) cells as a source for cell therapy materials. A source for mesenchymal stem cells could be obtained from the patient’s bone marrow. The cells would need to grow outside the body for several days in a facility like the Emory Personalized Immunotherapy Center to have enough for a therapeutic effect.