From Emory Medicine, Spring 2013
A small clinical study of clarithromycin for the sleep disorder hypersomnia shows that the antibiotic can combat patients’ subjective experience of sleepiness, but it does not seem to improve reaction time measured in a video-game-type vigilance task.
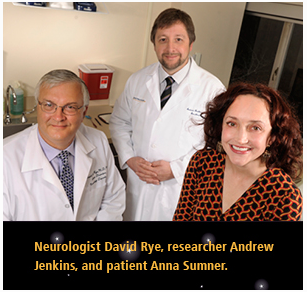
The effects of clarithromycin in hypersomnia were first observed by Emory doctors when a pioneering patient (Anna Sumner, whose story is told in this Emory Medicine article) unexpectedly experienced sleeplessness when taking it for a respiratory infection.
The results of the study were published online by Annals of Neurology on June 10.
Lynn Marie Trotti, MD, David Rye, MD, PhD and colleagues from the Department of Neurology and Emory Sleep Center conducted the study, which involved 23 patients.
Advantages of clarithromycin:
- It’s inexpensive and widely available.
- It’s an option for people dealing with hypersomnia for whom other medications, such as modafinil, are not helpful or tolerable.
- It represents an alternative to flumazenil, the benzodiazepine antidote that has been shown to help some hypersomnia patients. Flumazenil used to be very scarce, and shortages occur (Hypersomnia Foundation/American Society of Health System Pharmacists).
Disadvantages of clarithromycin:
- It’s an antibiotic, so it probably changes intestinal bacteria.
- Chronic use could promote the growth of antibiotic-resistant bacteria.
- Most patients reported an altered sense of taste or smell. Some describe this as a metallic mouth sensation.
Hypersomnia is a sleep disorder in which individuals feel frequent or constant sleepiness and need to sleep for long portions of the day (more than 70 hours per week). It is distinct from other sleep disorders such as narcolepsy and sleep apnea, but its prevalence is unclear.
Previous research at Emory has shown that many individuals with hypersomnia have a substance in their spinal fluid that acts like a sleeping pill, enhancing the action of the neurotransmitter GABA. Laboratory experiments have shown that clarithromycin acts similarly to flumazenil, in that it counteracts the GABA-enhancing substance from spinal fluid.
This was the first double-blind, placebo-controlled study of a drug targeting the GABA-enhancing mechanism in hypersomnia, instead of a “wake-promoting” medication such as modafinil. The study was performed in a crossover design: two weeks of either clarithromycin or control, with a week in between. The authors note that taste-alteration side effects may have made some participants aware of what they received.
All the patients in the study had “GABA-related hypersomnia” as verified by spinal tap. At the time of the study, participants could not be taking flumazenil, but they could be taking medications such as modafinil. Even so, with clarithromycin, participants reported an almost four point improvement on their Epworth Sleepiness Scale (from 14 to 10, on a scale from 0 to 24). The authors conclude:
“The benefit observed is large enough to be clinically meaningful, and is of the same magnitude or higher than that reported with modafinil in narcolepsy and shiftwork trials.”
Modafinil did generate a significant effect with hypersomnia patients (6 points on the same scale) in this 2014 study from Germany.
The Emory authors say there is a possibility that clarithromycin is acting as an anti-inflammatory or by modifying intestinal bacteria (since the microbiome influences the nervous system), rather than through GABA. More research could clear this up.
The authors have previously reported a survey of patients’ experiences with clarithromycin in hypersomnia and in Kleine-Levin syndrome. Trotti says that some hypersomnia patients have been taking clarithromycin for years, and in others, effectiveness wears off over time.

