Emory University played a key role in a landmark international study evaluating the safety and efficacy of the long-acting, injectable drug, cabotegravir (CAB LA), for HIV prevention.
The randomized, controlled, double-blind study found that cabotegravir was 69% more effective (95% CI 41%-84%) in preventing HIV acquisition in men who have sex with men (MSM) and transgender women who have sex with men when compared to the current standard of care, daily oral emtricitabine/tenofovir disoproxil fumarate 200 mg and 300 mg (FTC/TDF) tablets.
The study achieved its primary objective of non-inferiority with the difference approaching superiority in favor of cabotegravir, pending final analysis.
The findings were so positive that, during a planned review of study data, an independent Data and Safety Monitoring Board (DSMB) recommended the study results be announced as soon as possible. The study sponsor, the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, agreed with that recommendation.
Emory, through the Emory-CDC HIV Clinical Trials Unit, enrolled 7% of the study’s more than 4,500 worldwide participants at three of its clinical research sites: The Hope Clinic (86 participants) and the Ponce de Leon Center (35 participants) in Atlanta and at the CDC’s Silom Community Clinic in Bangkok, Thailand (203 participants).
“This is a landmark study with a new approach that will change how HIV prevention is being done and will open the field to future interventions,” says Carlos del Rio, MD, the executive associate dean, Emory University School of Medicine at Grady Health System. Del Rio is a member of the study team and the principal investigator at the Ponce de Leon Center.
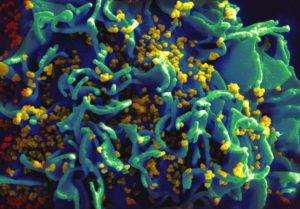
HIV-infected H9 T cell Scanning electron micrograph of HIV particles infecting a human H9 T cell, colorized in blue, turqoise, and yellow. Credit: NIAID
Colleen Kelley, MD, MPH, associate professor at Emory University School of Medicine, served as the principal investigator at Hope Clinic, which was the third-highest enrolling site in the United States.
“Having options and choice of HIV prevention products is critical,” says Kelley. “An injectable HIV prevention option may be ideal for people at elevated risk for HIV who don’t want to take pills or have trouble remembering to take a pill every day. They might now opt to have the injection every eight weeks instead. We look forward to the development of HIV prevention products in the future that require even less frequent dosing than every eight weeks.”
The study was one of the first-ever clinical trials to directly compare two active prevention agents head to head.
The HIV Prevention Trials Network (HPTN) announced the results from the study, known as HPTN 083, which enrolled enrolled 4,570 cisgender men and transgender women who have sex with men in Argentina, Brazil, Peru, Thailand, the United States, Vietnam and South Africa.
This study, in contrast to some prior studies, was successful in enrolling people from demographic risk groups at elevated risk of HIV infection. Two-thirds of study participants were under 30 years of age, and 12% were transgender women. Half of the participants in the United States identified as Black or African American.
Of the 50 people in the trial who acquired HIV, 12 were randomized to the long-acting cabotegravir arm and 38 were randomized to the daily, oral FTC/TDF arm – in other words, about three times the number of incident HIV infections were in the TDF/FTC arm than in the CAB arm.
Adherence to oral FTC/TDF was high, based on a random subset sampling that detected tenofovir (> 0.31 ng/ml) in 87% of all samples tested. Despite this high level of adherence to oral therapy, long-acting cabotegravir was 69% (95% CI 41%-84%) more effective than FTC/TDF in preventing HIV acquisition in the study population. However, it is notable that both interventions were highly effective in preventing new HIV infections.
The blinded, randomized portion of the study is now ending, and all participants are being informed of the results and will be told which study medication they received. Participants who were in the TDF/FTC arm will be offered CAB LA when it becomes available. Participants in the CAB LA arm will continue to receive it. Participants who do not want to receive CAB LA will be offered TDF/FTC.
The HPTN 083 study was jointly funded by NIAID and ViiV Healthcare. Study product is provided by ViiV Healthcare and Gilead Sciences, Inc.

