Chorioamnionitis is a complication of pregnancy: inflammation of the membranes surrounding the fetus, caused by a bacterial infection. It has the potential to inflict damage to the brain of the fetus, especially when combined with fetal hypoxia, and is a known risk factor for developing cerebral palsy.
Chia-Yi (Alex) Kuan and his team, who study fetal brain injury in the Department of Pediatrics, have a new paper in Journal of Neuroscience on a strategy for inhibiting fetal brain inflammation. Postdoctoral fellows Dianer Yang, Yu-Yo Sun and Siddhartha Kumar Bhaumik are co-first authors.
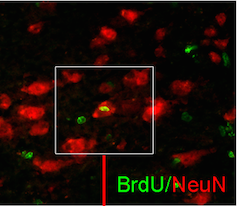
The researchers show that a type of immune cells called Th17 cells seems to be driving inflammation because the rest of the fetal immune system is still immature. A marker of Th17 cells is elevated in blood samples from human infants with chorioamnionitis, the researchers found. Th17 cells are thought to be important for both autoimmunity and anti-microbial responses.
A drug called fingolimod, which stops immune cells from circulating out of the lymph nodes, was effective in reducing inflammation-induced fetal brain injury in animal models. Fingolimod has been approved by the FDA for use with multiple sclerosis and has been studied in clinical trials of kidney transplantation. The authors write that it may be a potential add-on to hypothermia as a treatment for infants in danger of hypoxia + infection-induced brain damage.